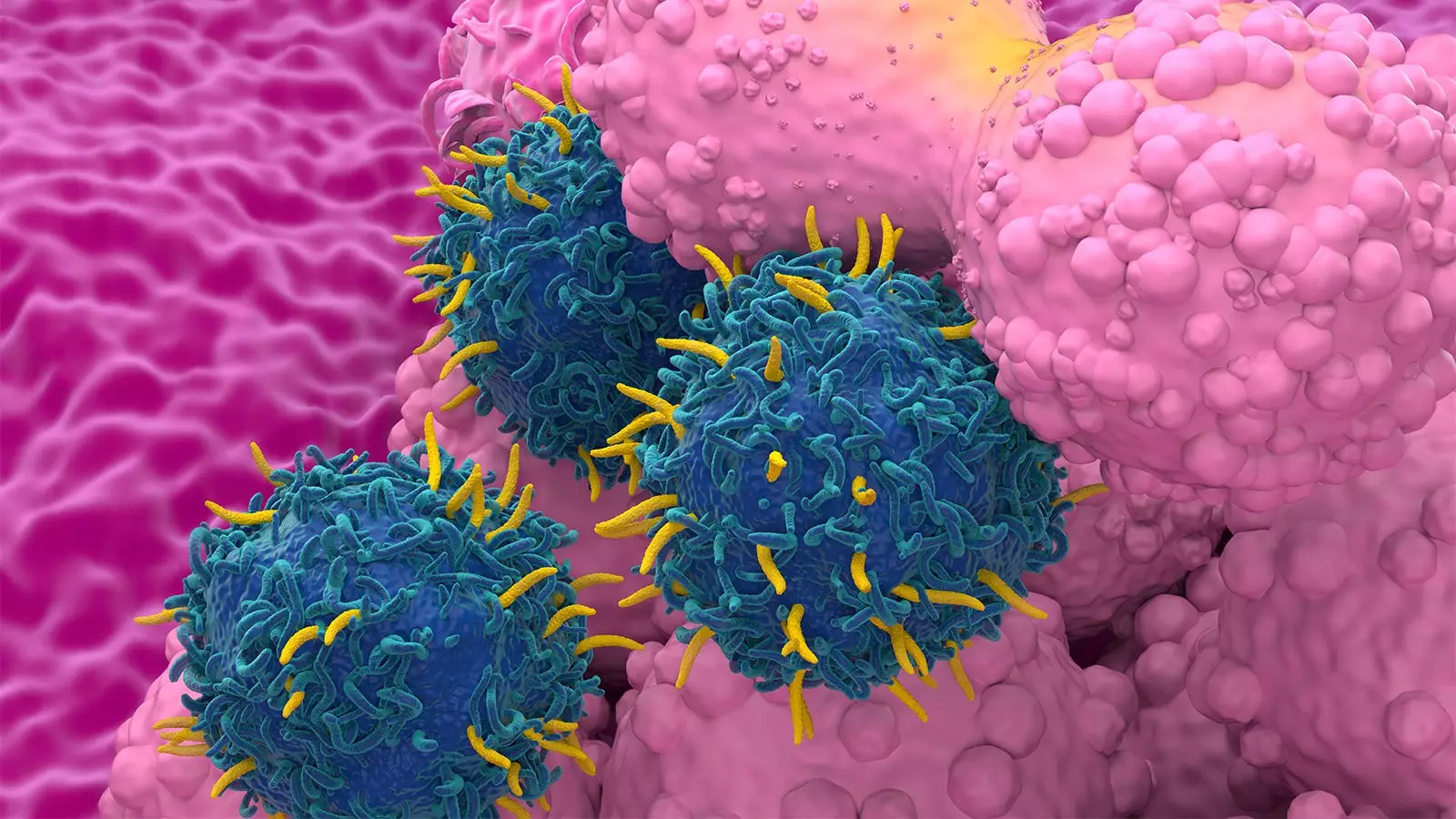
CAR T-cell therapy has been a revolutionary advancement in cancer treatment, offering new hope to patients with refractory or relapsed malignancies. However, recent concerns have been raised regarding the incidence of second primary malignancies (SPM) associated with this therapy. A systematic literature review and meta-analysis aimed to evaluate the risk of SPM with CAR T-cell therapy compared to standard-of-care (SOC) cancer therapies.
The analysis involved 5,517 patients with a median follow-up of 21.7 months and revealed a 5.8% rate of SPM. Surprisingly, the rate did not vary based on the type of disease treated or the specific CAR T-cell product used. Factors such as study setting (clinical trial vs. real-world experience), longer duration of follow-up, and the number of therapies administered prior to CAR-T treatment were associated with a higher risk of SPM. Notably, the analysis comparing CAR T-cell therapy to SOC treatments showed similar rates of SPM, questioning the perceived increased risk associated with CAR T-cell therapy.
The FDA’s announcement of an investigation into reports of secondary T-cell malignancies linked to CAR T-cell therapy raised significant concerns. However, it is crucial to consider potential biases in adverse event (AE) data reporting and accurately assess the risk of developing SPMs. Factors such as patient age, follow-up duration, initial diagnosis, and previous treatments should be carefully evaluated to contextualize the risk associated with CAR T-cell therapy.
The need for more long-term data to better understand the factors contributing to SPM risk is evident. Patients seek information and reassurance from healthcare providers regarding the safety of their treatment options. Interpreting data cautiously and providing context is essential to address patient concerns and ensure informed decision-making.
The systematic review included 18 clinical trials and seven real-world studies involving over 5,000 patients. Hematologic malignancies and solid tumors were the most common types of SPM observed, with a low incidence of T-cell malignancies. The association between follow-up duration and SPM rate highlights the importance of ongoing monitoring and survivorship considerations in CAR T-cell therapy.
While concerns regarding SPM risk with CAR T-cell therapy exist, the available evidence suggests that the risk is comparable to that of traditional cancer treatments. Factors unrelated to the therapy itself may contribute to the development of SPMs. Continued research, long-term monitoring, and patient education are essential to ensure the safety and effectiveness of CAR T-cell therapy in cancer treatment.

Leave a Reply