Axial Spondyloarthritis (axSpA) is a chronic inflammatory rheumatic disease primarily affecting the spine and the sacroiliac joints. It manifests in two forms: radiographic axSpA, often referred to as ankylosing spondylitis, and non-radiographic axSpA, which lacks definitive radiographic changes but presents with similar clinical symptoms. Patients across both categories frequently experience significant pain, stiffness, and functional impairment, leading to a diminished quality of life. The treatment landscape for axSpA has evolved, particularly for patients who exhibit inadequate responses to traditional therapies, specifically nonsteroidal anti-inflammatory drugs (NSAIDs).
NSAIDs are typically the first line of defense in managing axSpA due to their anti-inflammatory properties. However, not all patients derive benefit from NSAIDs, and some may experience intolerable side effects, thus necessitating alternate therapeutic avenues. When NSAIDs are ineffective or contraindicated, physicians must explore other pharmacological approaches, ensuring a robust response to manage the condition’s debilitating effects.
The guidelines released by the Assessment of SpondyloArthritis International Society and the European League Against Rheumatism (ASAS-EULAR) recommend combining both pharmacological and non-pharmacological strategies to optimize treatment. Physical therapy, lifestyle modifications, and patient education form essential components of a comprehensive treatment plan aimed at reducing pain and preventing disease progression.
With the advent of biologic therapy, the treatment paradigm for axSpA has experienced significant shifts. Tumor necrosis factor (TNF) inhibitors and Interleukin-17 (IL-17) blockers have emerged as vital alternatives for patients not adequately managed with NSAIDs. Treatments like adalimumab, infliximab, and secukinumab target inflammation more specifically and have been utilized with varying success.
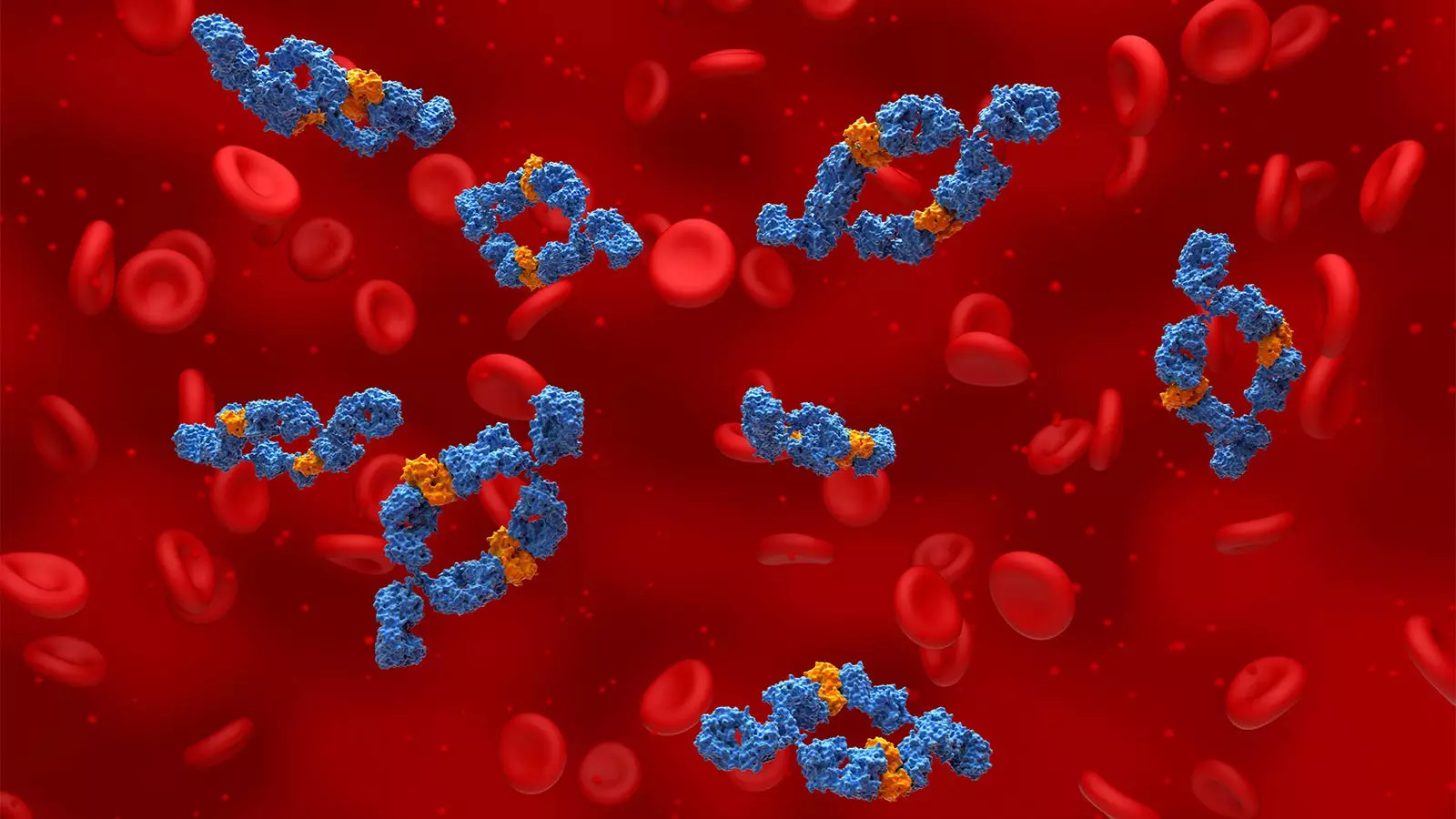
Recent advancements have introduced a novel biopharmaceutical that holds promise for axSpA patients: bimekizumab. This dual-targeted monoclonal antibody inhibits both IL-17A and IL-17F. Gaining FDA approval for active non-radiographic axSpA in September, bimekizumab has been widely celebrated in the rheumatology community. The BE-MOBILE studies have demonstrated notable efficacy in both forms of axSpA, providing a new strategy for patients who have previously struggled with treatment response.
An examination of the efficacy of bimekizumab reveals its impressive performance in clinical trials. In the BE-MOBILE 1 and BE-MOBILE 2 studies, roughly 45% to 48% of participants treated with bimekizumab achieved a 40% improvement in primary outcome measures by week 16, a significant difference compared to the placebo group. Long-term follow-ups indicated that over 60% of patients were still classified as responders after one year of treatment. Notably, patients transitioning from placebo to bimekizumab post-week 16 still achieved comparable outcomes, suggesting robust therapeutic potential.
As axSpA treatment options expand, understanding the nuances between TNF inhibitors and IL-17 inhibitors remains pivotal. Clinicians often choose between these therapies based on the presence of extra-articular manifestations, with IL-17 inhibitors typically being reserved for use when TNF inhibitors demonstrate limited effectiveness.
Evaluating New Horizons: JAK Inhibitors and Real-World Insights
The introduction of Janus kinase (JAK) inhibitors into the treatment milieu also reflects the innovation within the field. While data indicates that JAK inhibitors show promise, their effective use is often limited to patients with favorable cardiovascular profiles due to associated risks reported in clinical trials. Despite this, real-world analyses have revealed higher discontinuation rates for JAK inhibitors compared to TNF and IL-17 inhibitors, underscoring the necessity to carry out head-to-head studies to discern the optimal treatment strategies.
Furthermore, systematic reviews affording clarity on treatment responses have demonstrated that bimekizumab yields higher efficacy rates compared to secukinumab and aligns closely in efficacy with several other established therapies. The favorable safety profile of bimekizumab further positions it as a promising candidate in the expanding universe of axSpA treatments.
As research in axSpA continues to advance, healthcare providers are presented with an expanding toolbox of treatments that cater to the diverse needs of patients. The integration of bimekizumab into treatment protocols signifies not only a critical addition to the existing therapeutic arsenal but also an exciting step forward in enhancing patient outcomes for those grappling with the challenges of axial spondyloarthritis. With ongoing research and continued clinical vigilance, the future holds great potential for innovative therapies designed to improve quality of life and functional outcomes in affected patients.

Leave a Reply