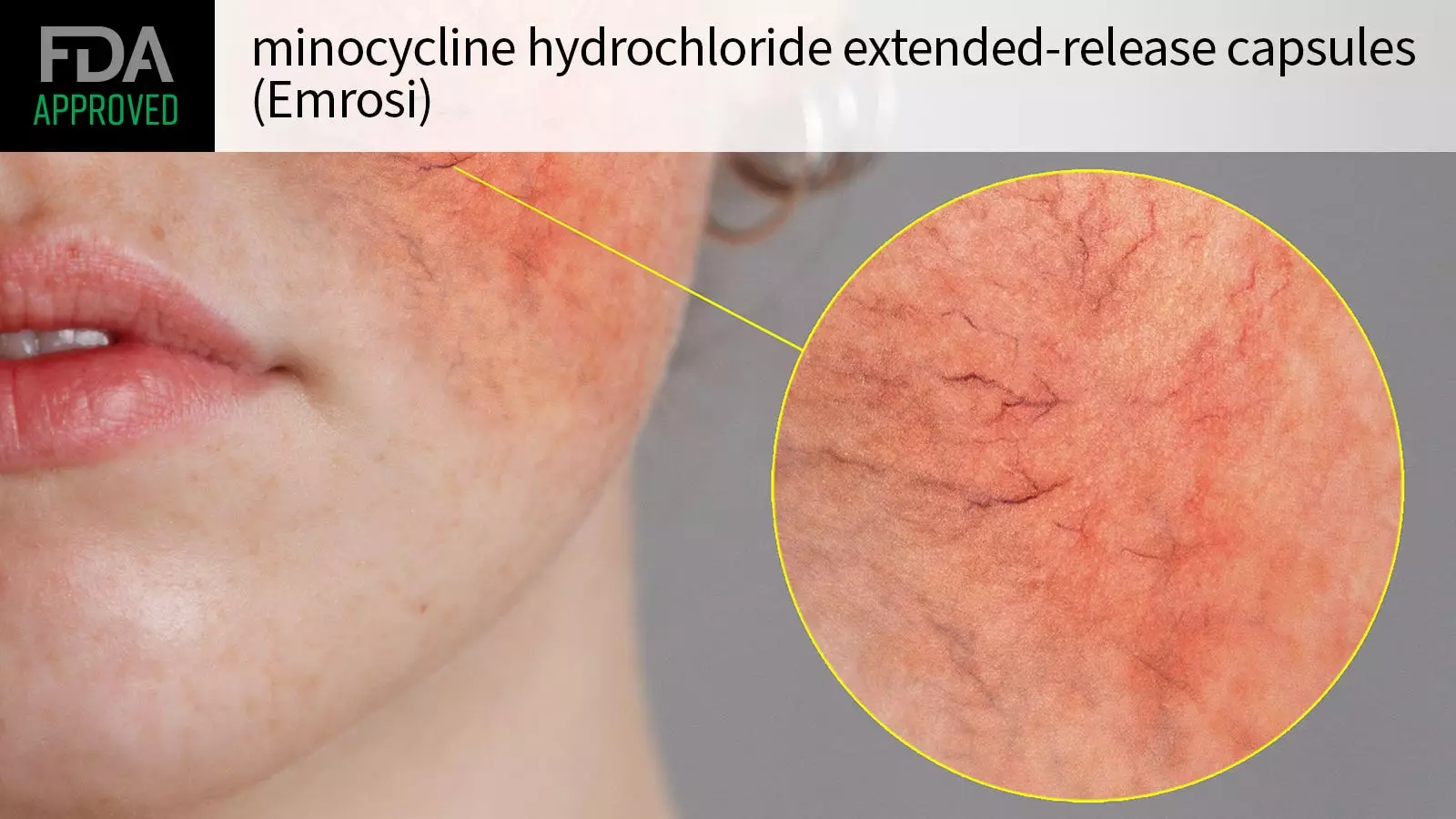
The recent approval of minocycline hydrochloride extended-release capsules—marketed under the name Emrosi—by the FDA marks a significant milestone in the treatment of rosacea. This decision is particularly noteworthy for individuals suffering from inflammatory lesions of rosacea, a chronic skin condition that can severely impact the quality of life. Developed by Journey Medical, this tetracycline antibiotic aims to provide a more efficient therapeutic option, building on earlier treatments that have been the standard of care for years.
This approval stems from robust clinical evidence derived from two multicenter phase III trials, designated MVOR-1 and MVOR-2, which engaged a total of 653 adult participants diagnosed with papulopustular rosacea. The structure of these studies showed a methodical approach, randomly assigning participants to receive either daily doses of minocycline hydrochloride (40 mg), doxycycline, or a placebo over 16 weeks. The primary goal was to determine the efficacy of the new formulation compared to existing treatments, setting the bar high with stringent baseline criteria.
Participants commenced the trials with considerable skin manifestations, averaging 25 inflammatory lesions and possessing moderate to severe disease indicators. This establishes the clinical relevance for those with considerable flare-ups who seek relief.
The results from these trials have been promising. In MVOR-1, a striking 65% of patients treated with minocycline hydrochloride achieved an Investigator’s Global Assessment (IGA) score of 0-1—indicating clear or near-clear skin—compared to 46% in the doxycycline group and 31% in those receiving a placebo. Likewise, MVOR-2 mirrored these findings with 60% efficacy for minocycline versus only 31% and 27% for doxycycline and placebo, respectively. Furthermore, mean reductions in inflammatory lesions, ranging from 75-79% in the minocycline group, outperformed both doxycycline and placebo, which reported reductions of 60-63% and 46-47% respectively. This data reinforces the effective potential of minocycline hydrochloride as a first-line treatment alternative.
While these results are encouraging, safety concerns are paramount in any new medication. The most noteworthy adverse event reported in clinical trials was dyspepsia, impacting 2% of patients versus none in the placebo cohort. Such occurrences necessitate a cautious approach to prescribing, aligning with FDA guidelines that recommend minocycline hydrochloride to be used judiciously to mitigate the risks associated with drug-resistant bacteria.
It’s crucial to highlight that the use of minocycline is contraindicated for individuals with a known hypersensitivity to tetracyclines. Additionally, reports have surfaced linking the antibiotic to severe side effects, including anaphylaxis and skin reactions, which can be life-threatening.
With this new approval, Journey Medical is poised to make minocycline hydrochloride available in the first half of 2025. For patients enduring the challenges imposed by rosacea, this development holds promise for improved management of their condition. However, as healthcare providers prepare to integrate this treatment into clinical practice, the need for adherence to safety protocols and informed patient consent remains unequivocally important. The road ahead involves thorough education about the drug’s benefits and potential risks to maximize patient safety and therapeutic success.

Leave a Reply