Herpes Simplex Virus Type 1 (HSV-1) is commonly recognized for causing cold sores, yet its influence extends far beyond superficial lesions. Recent studies have begun to illuminate HSV-1’s potential implications for neurological health, suggesting that this ubiquitous virus may be intricately linked to serious conditions such as Alzheimer’s disease. Recognizing that the virus can infiltrate the brain and central nervous system, researchers from the University of Colorado and the University of Bourgogne in France undertook an investigative study aimed at mapping the pathways and impacts of HSV-1 within the brain.
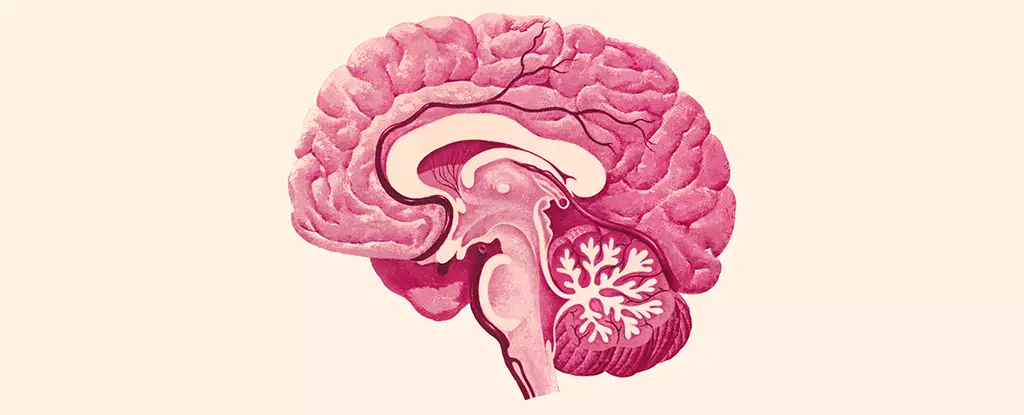
The introduction of HSV-1 into the central nervous system predominantly occurs through two major anatomical pathways: the trigeminal nerve and the olfactory nerve. Despite these established entry points, how the virus propagates within the confines of the brain has largely remained a mystery. Neurologist Christy Niemeyer emphasizes the importance of clarifying this pathway—understanding which brain regions are susceptible to infection is pivotal in deciphering the relationship between HSV-1 and neurodegenerative diseases.
The findings of the study revealed a striking pattern: HSV-1 predominantly targeted several critical areas of the brain, notably the brain stem and hypothalamus. The brain stem plays a crucial role in basic life functions, including regulating heart rate, respiration, and sleep cycles. The hypothalamus, meanwhile, governs a range of essential bodily functions from mood regulation to appetite control. In contrast, other pivotal areas such as the hippocampus—integral for memory processing—and the cortex—significant for attention and cognition—did not seem to harbor HSV-1 antigens, suggesting a selective vulnerability within the neural architecture.
A notable component of the study was its exploration of microglia, the innate immune cells housed in the central nervous system. These cells serve as a defense line against pathogens, yet can also mediate inflammation when activated. In response to HSV-1, the microglia in infected brain regions displayed marked inflammatory activity, which persisted even in the absence of the viral presence. This prolonged state of inflammation raises concerns about the potential for chronic neurodegeneration, even when overt symptoms of encephalitis—the severe inflammation of the brain—are absent.
Christy Niemeyer points out the significance of this ongoing immune response: “Even though the presence of HSV-1 is not causing full-blown encephalitis in the brain, it can still affect how these regions function.” This finding is a critical piece in the puzzle as it suggests that the mere presence of HSV-1 may have detrimental effects on neural functionality rather than only leading to overt illness.
The implications of HV-1 infection extend into the realm of neurodegenerative diseases, particularly Alzheimer’s. Recent hypotheses propose that the interplay between HSV-1 and microglia-induced inflammation could be a contributing factor to the onset and progression of Alzheimer’s disease. As researchers analyze the overlapping regions of the brain that are susceptible to both HSV-1 and Alzheimer’s pathology, the connections become increasingly intriguing.
Chronic inflammation, often triggered by persistent immune responses, has emerged as a known catalyst for various neurological and neurodegenerative conditions. The study’s findings deepen our understanding of how these viral infections might interact with underlying neurodegenerative processes. As Niemeyer states, “Persistently inflamed cells can lead to chronic inflammation, a known trigger for a number of neurological and neurodegenerative diseases.”
The recent research into HSV-1’s effects on the brain marks a significant advancement in our understanding of the potential ramifications of this seemingly benign virus. By elucidating the mechanisms through which HSV-1 accesses and impacts crucial brain areas, the study paves the way for further investigations into the connections between viral infections and neurodegenerative disorders. As science continues to uncover these relationships, it stands to reason that preventative strategies or therapeutic interventions could one day be developed to mitigate the effects of HSV-1 on brain health, potentially altering the course of diseases like Alzheimer’s that have long-term implications for millions globally.

Leave a Reply